Unfolding Prescription Drug Labeling Requirements
Bringing a prescription drug to market is like a jigsaw puzzle. The medication is the finished puzzle, but many pieces must be put in place before it’s complete. Packaging and sterility, for example, have nothing to do with the medication but are mandatory pieces. And then there are drug labeling requirements. For all the conversations industry shares, prescription drug and biological product labeling can be unfamiliar territory. But don’t let it be a missing piece.
What’s Under the Umbrella?
Many items reside under the umbrella of FDA human prescription drug labeling. Some labeling is written for medical professionals, some for patients and caregivers. There is content on the drug carton or bottle. Still more may be found as a packaging insert, and then the pages dispensed by the pharmacy. Most US FDA language relating to labeling is non-binding, with exceptions that are set forth under CFR statutes, described here.
Prescribing Information vs Patient Information
This is a dual-sided sheet. One side, “Prescribing Information” gives clinical and scientific data for physicians. The other side, “Patient Information,” educates patients/caregivers in plain language about the drug and how to take it. Prescribing Information is part of the FDA’s January 2006 final Physician Labeling Rule “PLR”. With that as background this article focuses on understanding patient/caregiver labeling.
Understanding Labeling Formats
Note the somewhat confusing but common use of “PI” to denote one of multiple meanings:
PI = Prescribing Information (for physicians)
PI = Patient Information
PI = Package Insert
And PPI = Patient Package Insert
The purpose of all forms of patient-facing content is to educate about the medicine and prevent possible adverse events from incorrect use. Formats include: IFU (Instructions for Use), PI (Patient Information), PPI (Patient Package Inserts) and MG (Medication Guides). Patients will likely receive all forms, regardless of redundancy. The titles sound similar, so what makes each distinct, and what is required vs. recommended? Let’s break them down.
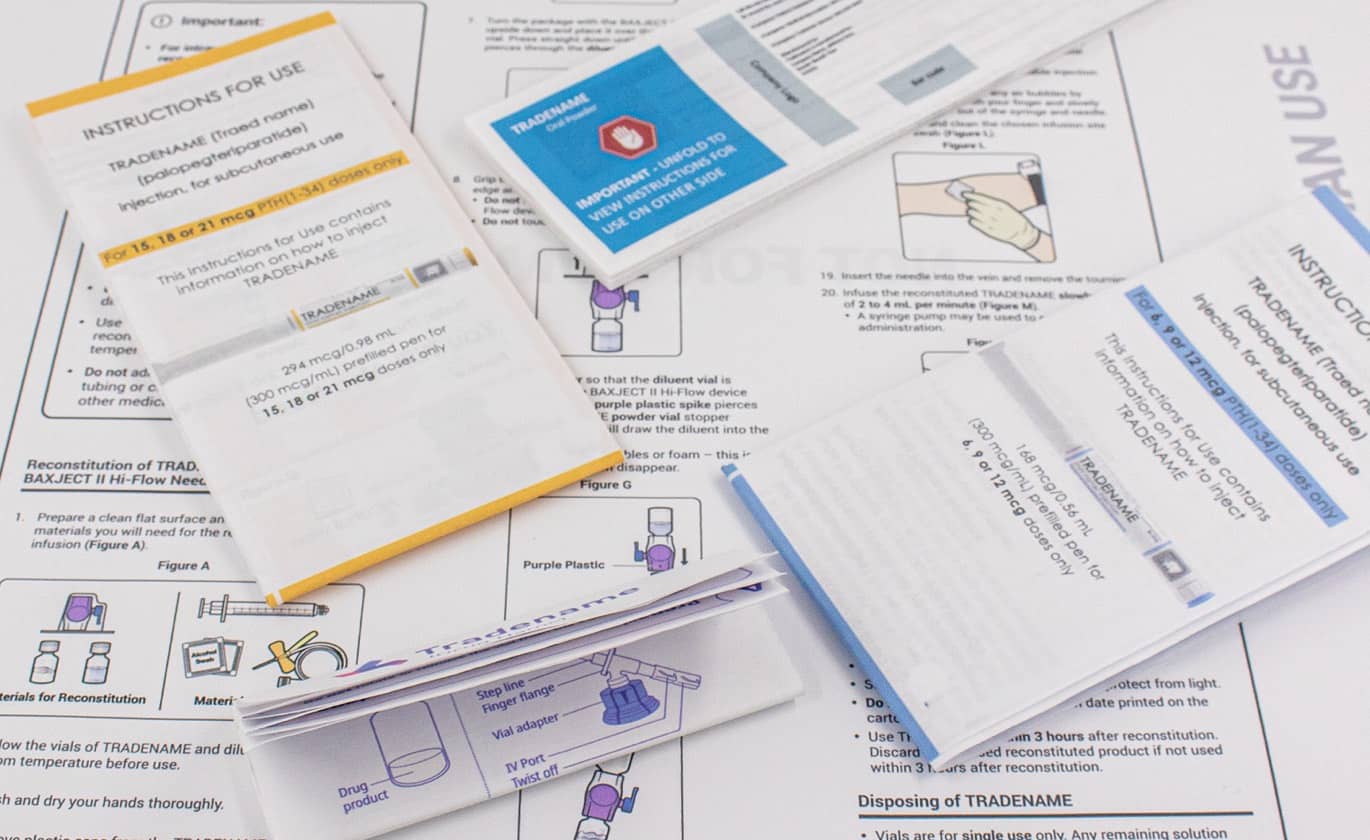
IFU: Instructions for Use. Not all medications call for IFUs. Current FDA input comes in the form of non-binding FDA Draft Guidance. Food and Drug Administration resources state, “The IFU is developed by applicants for patients who use drug products that have complicated or detailed patient-use instructions.” The IFU features patient friendly language, with step-by-step instructions (written and often with visual images to support), to encourage compliance. This includes steps if the medicine must be “prepared” (i.e., unwrapped, shaken, etc.), how to administer it (i.e., use of an inhaler, internal introduction to the body, etc.), storage and proper disposal. Dosage instructions, missed dosages, and other commonly encountered patient use scenarios should also be considered.
The bottom line of the IFU is to ensure patients use and handle medications properly. The IFU may also address different instructions for disparate patient groups, such as pediatric and adult. In determining whether a prescription drug application should include and IFU, the FDA suggests user-related risk analysis (URRA) and human factors studies. Additionally, the FDA expects consistency with IFU content to the corresponding Prescribing Information flier, although the IFU may include information that is not part of the PI.
PI: Patient Information. This “PI” encompasses both sides of the well-known (and rarely read) two-sided fold-out flier with the “Prescribing Information” side for physicians, and the “Patient Information” side for us. As with all forms, PI content tells the medicine’s purpose, what the drug should look like, warns who should not take the drug, how to take it, dosing, handling, storage.
PPI: Patient Package Insert. The Patient Package Insert is required for oral contraceptives and estrogen-containing products under 21 CFR 310.501 and 21 CFR 310.515. A PPI must also be prepared for drugs approved solely based on animal studies. In addition to basic information about its purpose and how to take it, PPIs include who should not take it, and side effects. The PPIs must be included every time the medication is dispensed. Drug companies may voluntarily include PPIs with other medications (without estrogen), also approved by the FDA. Voluntary PPIs are not required to be distributed to each patient.
MG: Medication Guide. Medical Guides also help end-users understand more about a medicine. The MG is distinct in that it applies only to products that come with significant “public health concerns.” Medical Guide requirements are found under 21 CFR 208. Unique to MGs, the FDA Amendments Act of 2007 (FDAAA) new section (505-1) directs the drug manufacturer to provide an MG. The section allows the FDA to compel a Risk Evaluation and Mitigation Strategy (REMS) to ensure the benefits of the drug outweigh risks. Content must include details about anything related to using the drug that must be followed to prevent serious adverse events. An MG might also be required if the medication will be ineffective unless the patient strictly follows certain protocols to ensure the drug performs as designed. The FDA may also call for an MG if patients may change their mind about whether to take the medicine when informed about potentially serious side effect(s).